Service Coordinators Helped Older Adults Who Live in Publicly Funded Housing Respond to COVID-19
While the COVID-19 pandemic has been especially difficult for older adults, a new Center report finds that service coordinators in publicly funded housing have helped older adult residents cope with the daunting challenges created by the pandemic. As part of the management team in affordable housing communities, service coordinators typically have education and experience in social work or human services. Their role is to advocate for effective service provision and to link older adults, people with disabilities, and low-income families to supportive services and community resources that promote independent, community-based living. In the report, which is based on a survey jointly conducted with the American Association of Service Coordinators (AASC), Jennifer Molinsky and I find that after the pandemic hit, many older residents struggled to meet personal and healthcare needs; obtain food, medication and supplies; and deal with the loneliness that resulted from the precautions necessary to protect them from the virus. The report documents the many ways service coordinators have responded to these problems such as helping residents access and use technology; facilitating procurement of needed resources; and developing new protocols and programs to help residents cope with isolation.
Service coordinators are placed in some affordable housing communities using either the property’s operating funds or through grants provided by HUD. They support financial and physical security, social connections, and the delivery of community-based services to older residents. To understand how their work changed during the pandemic, the Center partnered with AASC to distribute a survey to their 3,500 members between June and July of 2020. The 1,175 respondents worked on multifamily properties spanning 47 states as well as Washington, DC and Puerto Rico. About 3 of every 4 of the residents they supported were 62 years of age or older and 59 percent were dually eligible for Medicare and Medicaid.
Reflecting on the spring, service coordinators described interruptions in older adults’ support systems. Prior to the pandemic, service coordinators estimated that almost half of the older adults living on their properties relied on in-person assistance from agencies or friends and family to accomplish tasks such as housekeeping, laundry, or errands. About 3 out of 10 residents depended on a personal assistant to meet daily personal care needs such as dressing. COVID-19 interrupted these services: many properties restricted onsite access to reduce risks of virus transmission, some provider agencies instituted restricted visits to properties with COVID positive residents, and agencies also coped with new staffing challenges. In response, service coordinators knit together alternatives to create a safety net for residents, primarily by reaching out to informal family and volunteer supports and spending more time working with provider agencies to make temporary arrangements.
Without access to typical supports and transportation services, and with the need to avoid public spaces, it also became more difficult for older adults to procure food, medicine, and household supplies. Service coordinators estimated that 40 percent of residents did not have enough of these resources to isolate for a week. Service coordinators became more involved in helping residents fulfill these needs; 78 percent spent more time helping residents arrange the purchase or delivery of food, 46 percent were more involved with medications or medical supply acquisition, and 64 percent were more engaged in the purchase or delivery of household goods. A large amount of this effort was devoted to managing public benefits as well as relationships with food banks, churches, and other donor organizations, as well as coordinating the delivery and distribution of resources once procured.
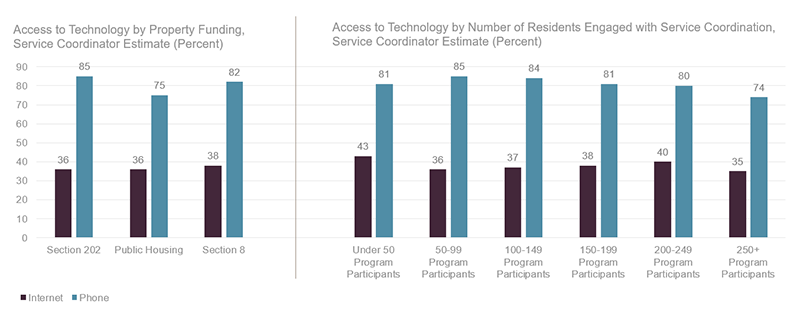
Medical care also changed radically during this period, with a new reliance on telehealth. At the time of the survey, half of service coordinators had spent more time facilitating virtual medical care, including both ensuring access to technology and supporting resident capacity to use the technology. They also acted as intermediaries to facilitate communication between medical professionals and residents who were unable to speak directly. Limited access to technology made the sudden shift to telemedicine, as well as other virtual platforms, particularly complicated. Survey respondents estimated that only 38 percent of residents had both internet service and an internet-capable device (Figure 1).
Figure 1: Few Residents Had Internet Access When the Pandemic Hit
Note: Properties that accept multiple funding sources are duplicated in this figure for each relevant funder. Also, participation in service coordinator programs is voluntary and count demonstrates number of participants, not size of the property.
Source: JCHS survey of 1,175 service coordinators conducted June 23, 2020 to July 17, 2020.
Service coordinators circumvented missing technology by helping residents complete benefits forms by hand or by using the telephone to conduct regular wellness checks to assess emerging needs. Ninety percent of them relied on the phone to communicate with residents and more than three quarters used written notices, fliers, and newsletters. Yet even for residents who had access to the internet, technological literacy was a barrier to healthcare, social support, and communication. Service coordinators managed technology issues and taught residents how to use various platforms ranging from video chat to the virtual public library. Many survey respondents noted that if they could hire extra help, they would devote time to building residents’ technology skills.
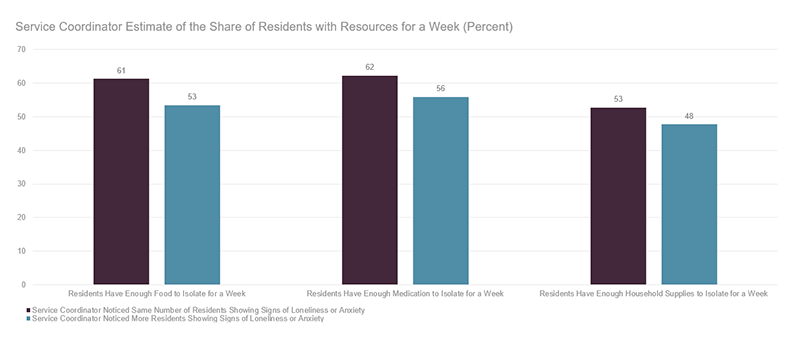
Without the typical group meals and other regular gatherings, the pandemic deeply impacted the social lives of residents. Service coordinators noticed more residents showing signs of anxiety and loneliness; as one noted, “[I have] observed residents who are sad and feeling desperate to socialize.” The many disruptions may have compounded these socio-emotional experiences as service coordinators were more likely to report increased loneliness and anxiety when fewer residents had the resources they needed to isolate for a week (Figure 2).
Figure 2: With Higher Resident Resource Deficits, Service Coordinators Observed More Residents Showing Signs of Loneliness or Anxiety
Source: JCHS survey of 1,175 service coordinators conducted June 23, 2020 to July 17, 2020.
Service coordinators focused their time addressing this loneliness and anxiety. In addition to referrals to professional mental health supports, they took measures to deepen their relationships with residents, created distanced celebrations, and distributed activities to help people cope with social isolation. They also modified community-building activities to promote connections at a distance, such as encouraging residents to personalize and decorate public spaces and visually engage with the property beyond their apartment walls or using physical spaces and message boards in creative ways. One posted community games on bulletin boards, “giving residents a reason to walk out of their apartment for exercise but keeping them close to home.” They also constructed social infrastructure, creating various forms of telephone-based peer support systems.
Service coordinators did identify outstanding needs. In addition to the digital divide, many assessed that residents would benefit from more professional mental health support. As the pandemic wears on, these challenges may be exacerbated by the length of isolation and weather-related limitations on outdoor gatherings. Public resources will shift, and families who have been providing care will return to in-person work, creating new gaps. Service coordinators themselves will also be impacted by the pandemic over time. They have extended their roles to meet emergent demands and many worry about burn out. Given their relationships with residents and residents’ families, as well as public and community organizations, service coordinators are uniquely positioned to expand older adult resilience during the COVID-19 crisis, but to do so, they will need additional and ongoing support, such as embedded nurses and expanded technology access for properties. Funding is also needed to place service coordinators in all eligible housing. Strategic investments will augment the efforts of service coordinators and help them perform their essential work.